Urinary incontinence
Highlights
Types of Urinary Incontinence
Urinary incontinence is generally categorized into the following types:
- Stress incontinence is triggered by activities (coughing, sneezing, laughing, running, or lifting) that apply pressure to a full bladder. Stress incontinence is very common among women, with childbirth and menopause increasing the risk for it. It can also affect men who have had surgical procedures for prostate disease, especially cancer.
- Urge incontinence, also called overactive bladder, is marked by a need to urinate frequently. There are many causes of urge incontinence, including medical conditions (benign prostatic hyperplasia, Parkinson’s disease, multiple sclerosis, stroke, and spinal cord injuries), surgeries (hysterectomy, radical prostatectomy), and infections.
- Overflow incontinence occurs when the bladder cannot empty completely, which leads to dribbling. Bladder obstruction and inactive bladder muscle can cause overflow incontinence. Risk factors include certain types of medications, benign prostatic hyperplasia, and nerve damage.
- Functional incontinence is incontinence due to mental or physical disabilities that impair a person’s ability to use or get to the toilet, despite a healthy urinary system.
- Mixed incontinence. Many people have more than one type of urinary incontinence.
Treatment of Urinary Incontinence
Treatment options for urinary incontinence depend on the type of incontinence and the severity of the condition. Treatments include:
- Lifestyle Changes. Significant weight gain can weaken pelvic floor muscle tone, leading to urinary incontinence. Losing weight through healthy diet and exercise is important. Regulating the time you drink fluids and avoiding alcohol and caffeine are also helpful.
- Behavioral Techniques. Pelvic floor exercises (Kegel exercises) can help strengthen the muscles of the pelvic floor that support the bladder and close the sphincter. Bladder training can help patients learn to delay urination.
- Medications. Drugs, such as oxybutynin (Ditropan, generic) and tolterodine (Detrol), are mainly used to treat urge incontinence.
- Surgery. Many types of surgical procedures are used to correct anatomical problems that contribute to severe urinary incontinence.
The American Urological Association’s 2012 guidelines for managing overactive bladder emphasize that behavioral therapies and lifestyle changes should be the first treatment approaches. According to a recent study, drugs for urge urinary incontinence only help about 20% of the women who take them and often have significant side effects.
Drug Approvals
- In 2012, the Food and Drug Administration (FDA) approved mirabegron (Myrbetriq), a new type of drug for treatment of overactive bladder.
- In 2011, the FDA approved Botox injections to treat urinary incontinence caused by neurological conditions such as spinal cord injury and multiple sclerosis.
Introduction
Urinary incontinence is the inability to control urination. It may be temporary or permanent, and can result from a variety of problems in the urinary tract. Urinary incontinence is generally divided into four types:
- Stress incontinence
- Urge incontinence
- Overflow incontinence
- Functional incontinence
Often, more than one type of incontinence is present. When this occurs, it is called mixed incontinence. Because incontinence is a symptom, rather than a disease, it is often hard to determine the cause. In addition, a variety of conditions may be the cause.
Normal Urination
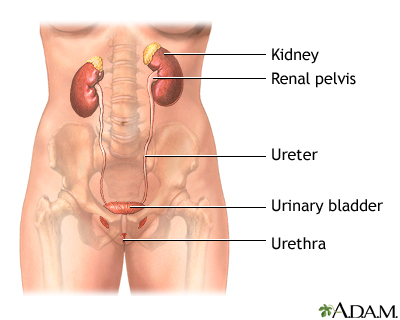
The urinary system helps to maintain proper water and salt balance throughout the body:
- The process of urination begins in the two kidneys, which process fluids and eliminate water and waste products to produce urine.
- Urine flows out of the kidneys into the bladder through two long tubes called ureters.
- The bladder is a sac that acts as a reservoir for urine. It is lined with a tissue membrane and enclosed in a powerful muscle called the detrusor. The bladder rests on top of the pelvic floor. This is a muscular structure similar to a sling running between the pubic bone in front to the base of the spine.
- The bladder stores the urine until it is eliminated from the body via a tube called the urethra, which is the lowest part of the urinary tract. (In men it is enclosed in the penis. In women it leads directly out.)
- The connection between the bladder and the urethra is called the bladder neck. Strong muscles called sphincter muscles encircle the bladder neck (the smooth internal sphincter muscles) and urethra (the fibrous external sphincter muscles).
The Process of Urination
The process of urination depends on a combination of automatic and voluntary muscle actions. There are two phases: the emptying phase and the filling and storage phase.
The Filling and Storage Phase. When a person has completed urination, the bladder is empty. This triggers the filling and storage phase, which includes both automatic and voluntary actions.
- Automatic Actions. The automatic signaling process in the brain relies on a pathway of nerve cells and chemical messengers (neurotransmitters) called the cholinergic and adrenergic systems. Important neurotransmitters include serotonin and noradrenaline. This pathway signals the detrusor muscle surrounding the bladder to relax. As the muscles relax, the bladder expands and allows urine to flow into it from the kidney. As the bladder fills to its capacity (about 8 - 16 oz of fluid) the nerves in the bladder send back signals of fullness to the spinal cord and the brain.
- Voluntary Actions. As the bladder swells, the person becomes conscious of a sensation of fullness. In response, the individual holds the urine back by voluntarily contracting the external sphincter muscles, the muscle group surrounding the urethra. These are the muscles that children learn to control during the toilet training process.
When the need to urinate becomes greater than one's ability to control it, urination (the emptying phase) begins.
The Emptying Phase. This phase also involves automatic and conscious actions.
- Automatic Actions. When a person is ready to urinate, the nervous system initiates the voiding reflex. The nerves in the spinal cord (not the brain) signal the detrusor muscle to contract. At the same time, nerves are also telling the involuntary internal sphincter (a strong muscle encircling the bladder neck) to relax. With the bladder neck now open, the urine flows out of the bladder into the urethra.
- Voluntary Actions. Once the urine enters the urethra, a person consciously relaxes the external sphincter muscles, which allows urine to completely drain from the bladder.
Stress Incontinence
The primary symptom of stress incontinence is leakage due to activities that apply pressure to a full bladder. High-impact exercise poses the greatest risk for leaking. But stress incontinence can occur with even minor activities, such as:
- Coughing
- Sneezing
- Laughing
- Running (sometimes even standing can produce leakage)
- Lifting
Leakage stops when the stress ends. If the leakage persists, it is more likely to be urge incontinence.
Causes of Stress Incontinence in Women
Stress incontinence occurs because the internal sphincter does not close completely. In both men and women, the aging process causes a general weakening of the sphincter muscles and a decrease in bladder capacity. However, the causes of stress incontinence may be different in men and women.
In women, stress incontinence is nearly always due to one or more of the following:
- Having had many children through vaginal deliveries. In such cases, pregnancy and childbirth strain and weaken the muscles of the pelvic floor causing a condition called urethral hypermobility. In urethral hypermobility the urethra does not close properly. It is one of the main causes of stress incontinence.
- Prolapsed uterus, in which the uterus protrudes into the vagina, occurs in about half of all women who have given birth. This condition can often cause incontinence.
- Estrogen deficiencies after menopause can cause the tissue lining the urethra to thin out so that the urethra may not close properly.
- Injury from surgery or radiation can cause stress incontinence. Injuries from previous surgeries can damage or weaken the bladder neck muscles.
Causes of Stress Incontinence in Men
Prostate treatments can impair the sphincter muscles and are major causes of stress incontinence in men.
Surgery or radiation for prostate cancer. Some degree of incontinence occurs in nearly all male patients for the first 3 - 6 months after radical prostatectomy. Within a year after the procedure, most men regain continence, although some leakage may still occur.
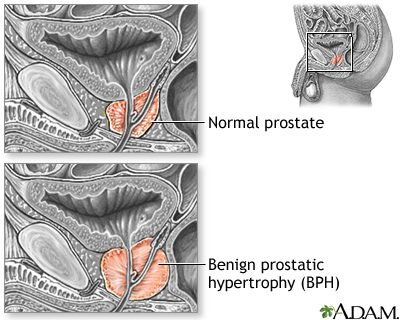
Surgery for benign prostatic hyperplasia. Stress incontinence can occur in some men after transurethral resection of the prostate (TURP), the standard treatment for severe benign prostatic hyperplasia (BPH).
Incontinence after prostate procedures is often a combination of urge and stress. Because studies often combine the two types of incontinence, it is not always clear which predominates.
Urge Incontinence
Urge incontinence (also called hyperactive, irritable, or overactive bladder) is the need to urinate frequently. People with overactive bladder may go to the bathroom more than 8 times over 24 hours, including two or more times a night, and have subsequent leakage. In some cases, urge incontinence occurs only at night. This is called nocturnal enuresis.
All cases of urge incontinence involve an overactive bladder. This occurs when the detrusor muscle, which surrounds the bladder, contracts inappropriately during the filling stage. When this happens, the urge to urinate cannot be voluntarily suppressed, even temporarily.
Conditions that can cause urge incontinence include:
- Benign prostatic hyperplasia (BPH), also called enlarged prostate
- Prostate surgical procedures including radical prostatectomy for prostate cancer and, less commonly, transurethral resection of the prostate (TURP) for BPH
- Hysterectomy, the surgical removal of the uterus
- Radiation to the pelvis that involves the bladder
- Damage to the central nervous system, which can occur from neurological conditions such as stroke, multiple sclerosis, Parkinson’s disease, or spinal cord or disk injury.
- Infections
- The aging process
- Emotional disorders such as anxiety
- Medications, including some sleeping pills
- Genetic factors may play a role in some cases
Overflow Incontinence
Overflow incontinence happens when the normal flow of urine is blocked and the bladder cannot empty completely. Overflow incontinence can be due to a number of conditions:
- A partial obstruction. In this case the urine cannot flow completely out of the bladder, so it never fully empties.
- An inactive bladder muscle. In contrast to urge incontinence (overactive bladder), with overflow incontinence the bladder is less active than normal, not more. It cannot empty properly and so becomes distended, or swollen. Eventually this distention stretches the internal sphincter until it opens partially and leakage occurs.
Causes of overflow incontinence include:
- Tumors
- Constipation
- Certain medications (such as anticholinergics, antidepressants, antipsychotics, sedatives, narcotics, and alpha-adrenergic blockers)
- Benign prostatic hyperplasia (enlarged prostate)
- Scar tissue
- Nerve damage. When nerves in the bladder are damaged the body cannot feel when the bladder is full and the bladder does not contract. Nerve damage can be caused by spinal cord injuries, previous surgery in the colon or rectum, or pelvic fractures. Diabetes, multiple sclerosis, and shingles also can cause this problem.
Functional Incontinence
Patients with functional incontinence have mental or physical disabilities that keep them from urinating normally, although the urinary system itself is structurally intact. Conditions that can lead to functional incontinence include:
- Parkinson's disease
- Alzheimer's disease and other forms of dementia. Mental confusion may prevent both recognition of the need to void and locating a bathroom.
- Severe depression. In such cases, people may become incontinent because they have difficulty with self-control.
Risk Factors
About 20 million American women and 6 million men have urinary incontinence or have experienced it at some time in their lives. The number, however, may actually be higher because many patients are often reluctant to discuss incontinence with their doctors.
Some of the main risk factors for urinary incontinence include:
- Female sex
- Older age
- Having given birth or having had prostate problems or prostate surgery
- Being overweight
- Neurological disorders (such as stroke or multiple sclerosis)
Gender
Urinary incontinence is far more common among women than men. This is because pregnancy and childbirth, menopause, and the anatomical shape of the female urinary tract all increase the risk for incontinence. For men, enlarged prostate and surgery to correct prostate problems are the main risk factors for urinary incontinence.
Age
As people age, the muscles in the bladder and urethrea weaken. For women, the loss of estrogen that occurs with menopause can also cause weakening of the pelvic and urinary tissues.
Pregnancy and Childbirth
Pregnancy and childbirth can increase the risk for stress incontinence. Vaginal birth can cause pelvic prolapse, a condition in which pelvic muscles weaken and the pelvic organs (bladder, uterus) slip into the vaginal canal. Pelvic prolapse, and the surgery used to correct it, can cause incontinence.
It is not clear if cesarean delivery helps prevent urinary incontinence. It’s also not clear if episiotomy prevents urinary incontinence. (Episiotomy is a surgical incision that is made during childbirth to the perineum, the muscle between the vagina and the rectum. Doctors perform this procedure to help widen the vaginal opening and prevent tearing.)
Weight
Being overweight is a major risk factor for all types of incontinence. The more a woman weighs, the greater her risk.
Lifestyle Factors
Diet. Acidic foods (citrus fruits, tomatoes, chocolate) and beverages (alcohol, caffeine) that irritate or overstimulate the bladder can increase the risk for incontinence. Spicy foods are also a problem. Excessive consumption of any type of fluid can create problems with incontinence but it’s also important not to cut back too much. Drinking insufficient amounts of healthy fluids (water) can lead to dehydration, which in turn causes bladder irritation and worsening of urinary incontinence.
Smoking. Smoking increases the risk for incontinence, especially in heavy smokers (more than a pack a day).
Exercise. High-impact exercise can trigger urinary leakage, particularly for women with a low foot arch. Shock to the pelvic area increases as the foot makes impact with hard surfaces. However, lack of physical exercise and movement can increase the risk for incontinence.
Smoking. Studies have reported a higher risk for incontinence, notably mixed incontinence, in women who are current or former heavy smokers (more than a pack a day).
Medical Conditions
Medical conditions associated with increased risk for urinary incontinence include:
- Stroke and spinal cord injury
- Neurological disorders (such as multiple sclerosis and Parkinson’s disease)
- Urinary tract infections
- Diabetes
- Kidney disease
- Constipation
- Enlarged prostate
- Restricted mobility
Medications
Drugs are often a cause of temporary incontinence.
- Alpha-adrenergic blockers, such as tamsulosin (Flomax), used for benign prostatic hyperplasia, can cause incontinence by over-relaxing the muscles.
- Alpha-adrenergic agonists, such as pseudoephedrine (found in some oral decongestants) tighten the muscles and may cause overflow incontinence.
- Diuretics, used for high blood pressure, often rapidly introduce high urine volumes into the bladder.
- Colchicine, a drug used for gout, can cause urge incontinence.
- Oral hormone replacement therapy (estrogen or estrogen plus progesterone) can increase the risk for urinary incontinence.
- Other medications and substances that increase the risk for incontinence are sedatives, muscle relaxants, antidepressants, antipsychotics, and antihistamines.
Complications
Emotional Effects
Urinary incontinence can have severe emotional effects. Patients may feel humiliated, isolated, and helpless about their condition. Incontinence can interfere with social and work activities. Depression is very common in women with incontinence. Incontinence also has emotional effects on men. A number of studies of patients with prostate cancer suggest that incontinence can be much more distressing side effect for men than erectile dysfunction (also a side effect of prostate cancer treatment).
Disruption of Daily Life
To prevent wetness or odors, people with incontinence may alter their way of life.
- Errands become very difficult and need advanced planning.
- Public bathrooms may be difficult to locate or unavailable. The problem is particularly severe for those with urge incontinence who have little time to reach a bathroom and have large volume spills.
Specific Effects of Incontinence in Seniors
Incontinence is particularly serious in older adults:
- Older adults who are otherwise healthy may stop exercising because of leakage, which can increase their impairment.
- Incontinence can result in loss of independence and quality of life.
- It is a major reason for nursing home placement.
- Severe incontinence may require catheterization. This is the insertion of a tube that allows urine to continually pass into an external collecting bag. Catheters can increase the risk for urinary tract infections and other complications.
- There is a strong association between urge incontinence and falls and injuries, which may be due in part to the rush to the toilet in the middle of the night. Keeping a pan or portable commode near the bed may prevent injuries as well as improve sleep and general convenience.
Diagnosis
To diagnose urinary incontinence, your doctor will first ask about your medical history and lifestyle habits (including fluid intake). The doctor will conduct a physical examination to check for possible conditions that may be contributing to the problem. The doctor may collect a urine sample for analysis to check for infection.
If further evaluation is required, more specialized tests (urodynamic studies) may be performed. Urodynamic studies are used to test how well the bladder and urethra are performing. These tests include postvoid residual urine volume, cystometry, uroflowmetry, cystoscopy, and electromyography. Imaging tests (video urodynamic tests) may also be used.
Medical History
The first step in the diagnosis of incontinence is a detailed medical history. The doctor will ask questions about your present and past medical conditions and patterns of urination. Be sure to let your doctor know:
- When the problem began
- Frequency of urination
- Amount of daily fluid intake
- Use of caffeine or alcohol
- Frequency and description of leakage or urine loss, including activity at the time, sensation of urge to urinate, and approximate volume of urine lost
- Frequency of urination during the night
- Whether the bladder feels empty after urinating
- Pain or burning during urination
- Problems starting or stopping the flow of urine
- Forcefulness of the urine stream
- Presence of blood, unusual odor or color in the urine
- A list of major surgeries with their dates, including pregnancies and deliveries, and other medical conditions
- Any medications being taken
Another method of diagnosing incontinence uses a test that asks 3 questions, which help a doctor distinguish between urge and stress urinary incontinence:
- During the last 3 months, have you leaked urine (even a small amount)?
- When did you leak urine? (During physical activity; when you could not reach the bathroom quickly enough; without physical activity or bladder urge.)
- When did you leak urine most often? (Physical activity; bladder urge; without or about equally with physical activity or bladder urge.)
Voiding Diary. You may find it helpful to keep a diary for 3 - 4 days before the office visit. This diary, sometimes referred to as a voiding diary or log, should be a detailed record of:
- Daily eating and drinking habits
- The times and amounts of normal urination
For each incident of incontinence, the log should also detail:
- The amount of urine lost (your doctor may ask you to collect and measure urine in a measuring cup during a 24-hour period)
- Whether the urge to urinate was present
- Whether you were involved in physical activity at the time
Physical Examination
Your doctor will do a thorough physical examination, checking for abnormalities or enlargements in the rectal, genital, and abdominal areas that may cause or contribute to the problem.
Postvoid Residual Urine Volume
The postvoid residual (PVR) urine volume test measures the amount of urine left after urination. Normally, about 50 mL or less of urine is left. More than 200 mL is abnormal. Amounts between 50 - 200 ml may require additional tests for interpretation. The most common method for measuring PVR is with a catheter, a soft tube that is inserted into the urethra within a few minutes of urination. Ultrasound, which is non-invasive, may also be used.
Cystometry
Cystometry, also called filling cystometry, measures how much urine the bladder can hold and the amount of pressure that builds up inside the bladder as it fills. Cystometry can be performed at the same time as the PVR test. The procedure uses several small catheters:
- A double-channel catheter is inserted through the urethra and into the bladder. It is used to fill the bladder with water and to measure pressure. Another catheter is inserted into the rectum or vagina, which is used to measure abdominal pressure.
- During the procedure, the patient informs the doctor about how the pressure is affecting the need to urinate..
- The patient may be asked to cough or strain to evaluate changes in bladder pressure and signs of leakage.
- A low leak point pressure measurement is a sign of stress incontinence.
The detrusor muscle of a normal bladder will not contract during bladder filling. Severe contractions at low amounts of administered fluid indicate urge incontinence. Stress incontinence is suspected when there is no significant increase in bladder pressure or detrusor muscle contractions during filling, but the patient experiences leakage if abdominal pressure increases.
Uroflowmetry
To determine whether the bladder is obstructed, an electronic test called uroflowmetry measures the speed of urine flow. To perform this test, the patient urinates into a special measuring device.
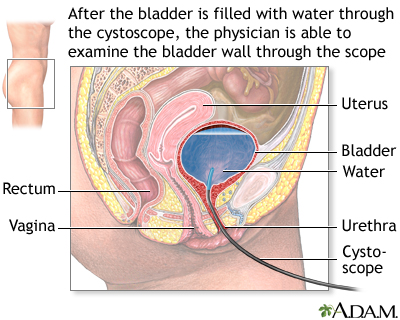
Cystoscopy
Cystoscopy, also called urethrocystoscopy, is performed to check for problems in the lower urinary tract, including the urethra and bladder. The doctor can determine the presence of structural problems including enlargement of the prostate, obstruction of the urethra or neck of the bladder, anatomical abnormalities, or bladder stones. The test may also identify bladder cancer, and causes of blood in the urine and infection.
In this procedure, a thin tube with a light at the end (cytoscope) is inserted into the bladder through the urethra. The doctor may insert tiny instruments through the cytoscope to take small tissue samples (biopsies). Cytoscopy is typically performed as an outpatient procedure. The patient may be given local, spinal, or general anesthesia.
Electromyography
Electromyography, also called electrophysiologic sphincter testing, is performed if the doctor suspects that nerve or muscle problems may be causing urinary incontinence. The test uses special sensors to measure electrical activity in the nerves and muscles around the sphincter. The test evaluates the function of the nerves serving the sphincter and pelvic floor muscles as well as the patient’s ability to control these muscles.
Video Urodynamic Tests
Video urodynamic testing combines urodynamic tests with imaging tests like ultrasound or a special type of x-ray procedure called fluoroscopy. Fluoroscopy involves filling the bladder with a contrast dye so that the doctor can examine what happens when the bladder is filled and emptied.
Ultrasound is a painless test that uses sound waves to produce images. With ultrasound, the bladder is filled with warm water and a sensor is placed on the abdomen or inside the vagina to look for structural problems or other abnormalities.
Treatment
Treatment for temporary incontinence can be rapid, simple, and effective. If urinary tract infections are the cause, they can be treated with antibiotics. Any related incontinence will often clear up in a short time. Medications that cause incontinence can be discontinued or changed to halt episodes.
Chronic incontinence may require a variety of treatments, depending on the cause. Treatment options are listed below in the order in which they are usually tried, from least-to-most invasive:
- Behavioral techniques, which include pelvic floor (Kegel) exercises and bladder training, are sometimes all a person needs for achieving continence. Behavioral techniques are helpful for both women and men. A number of devices can also be used to strengthen muscles and prevent urine leakage. Lifestyle modifications include changes to diet and fluid intake.
- Medications are tried next. Often, these involve anticholinergics.
- Surgery is the last resort. There are many effective surgical procedures for stress incontinence.
Lifestyle techniques to improve quality of life and improve hygiene are part of all treatments.
General Approach for Treating Specific Forms of Incontinence
Lifestyle measures, including dietary recommendations, bladder training, and continent aids, are useful for anyone with incontinence. Other treatments vary depending on whether the patient has stress or urge incontinence. In people who have both (mixed incontinence), the treatment usually is aimed at the predominant form.
Treating Stress Incontinence. The general goal for patients with stress incontinence is to strengthen the pelvic muscles. Typical steps for treating women with stress incontinence are:
- Behavioral techniques and noninvasive devices, including Kegel exercises, weighted vaginal cones, and biofeedback.
- Devices and continent aids for blocking urine in the urethra (vaginal pessaries, adhesive pads, and others).
- Medications may be used for stress incontinence (although not as often as for urge incontinence). Certain types of antidepressants (duloxetine, imipramine) are the main medications used for stress incontinence.
- Surgery is an option if symptoms do not improve with noninvasive methods. There are many surgical techniques. Most are designed to restore the bladder neck and urethra to their anatomically correct positions.
Treating Urge Incontinence. The goal of most treatments for urge incontinence is to reduce the hyperactivity of the bladder. The following methods may be helpful:
- Behavioral methods and lifestyle modification
- Medications (anticholinergics are the main type of drugs used)
- Procedures that stimulate the pelvic floor or nerves in the tailbone (the sacral nerves), which help retrain the bladder
Behavioral Treatments
With the exception of functional incontinence, most cases of incontinence will almost always improve with behavioral techniques. There are a variety of methods, but the focus is usually on strengthening or retraining the bladder. These exercises are very effective for women, and even for men recovering from surgery for prostate cancer.
Combination of Kegel Exercises and Bladder Training
Pelvic floor (Kegel) exercises and bladder training are often recommended as the first-line approach for treating all forms of urinary incontinence. They can help to substantially improve symptoms in many patients, including elderly people who have had the problem for years.
Pelvic Floor Muscle (Kegel) Exercises. Kegel exercises are designed to strengthen the muscles of the pelvic floor that support the bladder and close the sphincters.
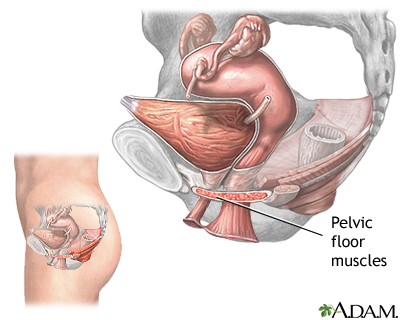
Dr. Kegel first developed these exercises to assist women before and after childbirth, but they are very useful in helping to improve continence for both men and women.
The general approach for learning and practicing Kegel exercises is as follows:
- Since the muscles are sometimes difficult to isolate, the best method is to first learn while urinating. The patient begins to urinate and then contracts the muscle in the pelvic area with intention of slowing or stopping the flow of urine. Women should contract the vaginal muscles as well. They can detect this by inserting a finger inside the vagina. When the vaginal walls tighten, the pelvic muscles are being correctly contracted. Patients should place their hands on their abdomen, thighs, and buttocks to make sure there is no movement in these areas while exercising.
- An alternate approach is to isolate the muscles used in Kegel contractions by sensing then squeezing and lifting the muscles in the rectum that are used in passing gas. (Again, women should contract the vaginal muscles as well.)
- The first method is used for strengthening the pelvic floor muscles. The patient slowly contracts and lifts the muscles and holds for 5 seconds, then releases them. There is a rest of 10 seconds between contractions.
- The second method is simply a quick contraction and release. The object of this exercise is to learn to shut off the urine flow rapidly.
- In general, patients should perform 5 - 15 contractions, three to five times daily.
Bladder Training. Bladder training involves a specific and graduated schedule for increasing the time between urinations:
- Patients start by planning short intervals between urinations, then gradually progressing with a goal of voiding every 3 - 4 hours.
- If the urge to urinate arises between scheduled voidings, patients should remain in place until the urge subsides. At the time, the patient moves slowly to a bathroom.
Vaginal Cones
This system uses a set of weights to improve pelvic floor muscle control:
- The typical set includes five cones of graduated weights ranging from 20 grams (less than 1 ounce) to 65 grams (slightly over 2 ounces).
- Starting with the lightest, the woman places the cone in her vagina while standing and attempts to prevent the cone from falling out. The muscles used to hold the cone are the same ones needed to improve continence.
As with standard Kegel exercises, frequent repetition is required, but most women will eventually be able to use the heavier weights and build up the ability to prevent stress and urge incontinence.
Biofeedback Devices
Women who are unable to learn Kegel muscle contraction and release with verbal instructions may be helped with the use of biofeedback:
- Biofeedback uses a vaginal or rectal probe inserted by the patient that relays information to monitoring equipment.
- The patient isolates the pelvic floor and bladder muscles and performs Kegel exercises.
- The monitor emits auditory or visual signals that indicate how strongly the patient is contracting the proper pelvic floor muscles and how effectively the bladder muscles are being released.
- The apparatus is designed for home use.
As with any Kegel exercise regimen, biofeedback must be used for several months before it is effective. Biofeedback that teaches control of pelvic muscles may also be helpful for children who have daytime wetting, frequent urinary tract infections, or both.
Medications
Medications for treating urinary incontinence increase sphincter or pelvic muscle strength or relax the bladder, improving the ability to hold more urine. Medications may be prescribed for both urge and stress incontinence, but they are generally most helpful for urge incontinence (overactive bladder). Because these drugs can cause side effects, it’s important to first try Kegel exercises, bladder training, and lifestyle modification methods.
Anticholinergics
Anticholinergics by relaxing the bladder muscle and preventing bladder spasms that signal the urge to urinate. They also increase the amount of urine the bladder can hold.
These drugs can produce small but significant improvements. However, they can have distressing side effects, notably dry mouth. Some studies indicate that the modest benefits of these drugs may not be outweighed by their side effects.
Anticholinergics include:
- Propantheline (ProBanthine, generic). This drug used to be the most commonly prescribed anticholinergic, but has been largely replaced by newer anticholinergics with fewer side effects.
- Oxybutynin (Ditropan, Oxytrol, generic)
- Tolterodine (Detrol)
- Hyoscyamine (Levbid, Hyomax, generic)
- Trospium (Sanctura, generic)
- Darifenacin (Enablex)
- Solifenacin (Vesicare)
- Fesoterodine (Toviaz)
Extended-release forms of oxybutynin (Ditropan XL) and tolterodine (Detrol LA) are available. They improve continence and have fewer adverse effects than short-acting forms. A skin patch form and topical gel form of oxybutynin (Oxytrol) is another option. They may have fewer side effects, such as dry mouth and constipation, than the pill form. Oxybutynin is also approved for pediatric use in children ages 6 and older.
Side effects of anticholinergic drugs include:
- Dry eyes (a particular problem for people who wear contact lenses; patients who wear contacts may wish to start with low doses of medication and gradually build up)
- Dry mouth
- Headache
- Constipation
- Rapid heart rate
- Confusion, forgetfulness, and possible worsening of mental function, particularly in older people with dementia, such as those with Alzheimer's disease
- Hallucinations, possibly, especially for children and older adults; doctors should monitor patients for this symptom
Alpha-Blockers
Alpha-blockers are drugs that relax smooth muscles and improve urine flow. They are useful for men with benign prostatic hyperplasia (BPH), also called enlarged prostate, who also have urge incontinence. The older alpha-blockers terazosin (Hytrin, generic) and doxazosin (Cardura, generic) are now prescribed less often than the newer selective alpha-blockers tamsulosin (Flomax, generic), alfuzosin (Uroxatral), and silodosin (Rapaflo). Alpha-blockers are sometimes combined with anticholinergics to treat men with moderate-to-severe lower urinary tract symptoms, including overactive bladder.
Antidepressants
Both urge and stress incontinence are affected in part by chemical messengers in the brain (neurotransmitters) that affect pathways involved with urination. Antidepressants that target serotonin, norepinephrine, or noradrenaline neurotransmitters are sometimes used for urge incontinence and may also be helpful for some people with stress incontinence.
- Imipramine (Tofranil, generic) is the main tricyclic antidepressant prescribed for urge, stress, or mixed incontinence. Tricyclic antidepressants act as anticholinergic drugs to relax the bladder muscle and ease spasms as well as tighten the sphincter. Like all tricyclic antidepressants, imipramine can cause side effects like sleepiness and dry mouth as well as more serious side effects like abnormal heart rate or rhythm (arrhythmia). In some people, imipramine can cause urinary retention.
- Duloxetine (Cymbalta) is an antidepressant that targets the neurotransmitters serotonin and norepinephrine, which are thought to play key roles in the normal action of bladder muscles and nerves. Duloxetine is not approved in the U.S. for stress urinary incontinence, but it is sometimes prescribed off-label for this condition. Common side effects may include constipation or diarrhea, sleepiness, dry mouth, and headache.
Other Drugs
Mirabegron (Myrbetriq). Mirabegron is a new, first-in-class drug that was approved in 2012 for treatment of overactive bladder. It works in a different way than anticholinergics and other drugs used for urinary incontinence. This drug can increase blood pressure and may cause urinary retention in some patients especially those with bladder outlet obstruction.
Botox. In 2011, the FDA approved onabotulinumtoxinA (Botox) injections to treat a specific type of urinary incontinence that occurs in people who have neurological conditions (such as spinal cord injury and multiple sclerosis) that cause overactive bladder. The injection is administered during a cystoscopy procedure.
Topical Estrogen. For some women whose urinary incontinence is associated with menopause, topical estrogen may help improve urinary incontinence and overactive bladder symptoms. The estrogen is administered vaginally using a cream, tablet, or ring. Oral estrogen replacement should not be used to treat urinary incontinence because it can worsen the condition.
Alpha-Adrenergic Agonists. Alpha-adrenergic agonists, such as clonidine (Catapres, generic), may be helpful for select patients with mild stress incontinence but they can have significant side effects and are not often prescribed.
Surgery
There are nearly 200 surgical procedures for incontinence. Most are designed to restore the bladder neck and urethra to their anatomically correct positions in patients with stress incontinence. Injections of bulking materials are another option for women and men.
The choice of surgical procedure depends on a number of factors, including the presence of bladder or uterine prolapse, the severity of incontinence, and the surgeon’s experience in performing specific types of surgery.
In general, patients should weigh all options carefully. They should discuss the situation with their doctor, and ask about their surgeon's experience. They should also be completely informed about the benefits and risks of the procedures. Patients will need to have a complete diagnostic evaluation with urodynamic testing before any surgical procedure.
Sling Procedures
A sling procedure is usually the first-line surgical approach for stress incontinence in women. It may also be useful for managing female urge incontinence. Sling procedures are also used for men who experience incontinence after prostatectomy.
The purpose of a sling procedure is to create a sling or hammock around the neck of the bladder to help keep the urethra closed. There are different types of sling procedures. They include:
- Suburethral, which is the traditional type
- Midurethral, which includes retropublic transvaginal tape (TVT) and transobturator tape (TOT)
Suburethral Sling Procedure. The suburethral, also called pubovaginal, sling is the traditional sling procedure. It uses a sling made from the patient’s own tissue (fascia), animal tissue, or a synthetic material. Suburethral means “beneath the urethra.” The procedure may be performed with laparoscopic or conventional “open” surgery. The procedure generally works as follows:
- The surgeon makes an incision above the pubic bone and removes a layer of abdominal fasci (tissue that covers muscle fibers). This muscle strip is set aside and later serves as the sling.
- The surgeon makes an incision in the vaginal wall. The piece of muscle fiber or material is attached under the urethra and bladder neck, somewhat like a hammock, and secured to the abdominal wall and pelvic bone.
- This sling then compresses the urethra back to its original position. The sling must be supportive without being too tense, which can cause urinary obstruction.
Complications can include infection, bleeding, and the formation of fistulas (holes that form and are usually infected).
Midurethral Sling Procedures. Midurethral sling procedures use slings made from synthetic mesh materials that are placed midway along the urethra. This newer type of sling procedure has become more commonly used than the conventional suburethral procedure because it can be performed on an outpatient basis using minimally invasive surgical techniques and no abdominal incisions.
There are two types of midurethral slings:
- In the retropublic procedure, the surgeon makes a small vaginal incision under the urethra and then two small incisions above the pubic bone.
- The transobturator procedure uses only a vaginal incision.
Sling Procedures in Men. For some men who have prostatectomy-induced incontinence, sling procedures may be a good option. Researchers have reported success rates similar to those of the artificial urinary sphincter, which is the standard surgical treatment for such patients. The sling procedure may be less effective for men who have undergone radiation therapy for prostate cancer. Minimally invasive procedures are also being tested.
Effectiveness and Complications. The sling procedure and the Burch colpsuspension seem to have similar success rates. Post-operative urinary problems, such as voiding problems, common urinary tract infections, and urge incontinence may occur. The FDA has reported complications associated with some synthetic mesh slings.
Retropubic Colposuspension (Burch Colposuspension)
Retropubic colposuspension aims to correct the position of the bladder and urethra by sewing the bladder neck and urethra directly to the surrounding pelvic bone or nearby structures.
Burch colposuspension is the standard approach. [Marshall-Marchetti Krantz (MMK) is an alternative approach.] It is often performed during abdominal surgeries such as hysterectomy or hernia operations. It is also performed along with sacrocolpopexy, a surgical procedure used to repair pelvic organ prolapse. (Pelvic organ prolapse occurs when the uterus or bladder slips from the pelvic cavity into the vagina. It is often due to pelvic muscle weakness that develops after childbirth.) Prolapse can lead to stress incontinence. However, prolapse surgery itself sometimes causes incontinence.
The Burch colposuspension procedure may be performed using open surgery or laparoscopy using spinal or general anesthesia. The surgeon makes an abdominal incision and secures the urethra and bladder neck with lateral (sideways) sutures that pass through thick bands of muscle tissue running along the pubic bones.
Effectiveness and Complications. Patients may stay in the hospital for a few days and usually need to use a urinary catheter for about 10 days after surgery. Because colposuspension surgery involves an abdominal incision, it can take up to 6 weeks for full recovery. (Laparoscopic procedures have a faster recovery time than open surgery.)
Complications can include problems with wound healing and postoperative voiding function. Convalescence time is longer with retropubic colposuspension than with sling procedures.
Artificial Sphincter
In cases of sphincter incompetence, or complete lack of sphincter function, an artificial internal sphincter may be implanted. This procedure is generally used for men, such as those who have experienced incontinence following radical prostatectomy.
This device uses a balloon reservoir and a cuff around the urethra that is controlled with a pump. The patient opens the cuff manually by activating the pump. The urethra opens and the bladder empties. The cuff closes automatically several minutes later. The two major drawbacks of the internal sphincter implant are malfunction of the implant and risk of infection.
Bulking Material Injections
Injections of materials, such as collagen, that provide bulk to help support the urethra may help the following patients:
- Women with severe stress incontinence who cannot or do not wish to have surgery that involves anesthesia.
- Men who have slight incontinence caused by prostate surgery procedures such as transurethral resection of the prostate (TURP) or radical prostatectomy (removal of the prostate gland in prostate cancer).
The Procedure.
- The basic procedure involves injecting bulking material into the tissue surrounding the urethra.
- The material used is usually animal or human collagen. (Collagen is the basic protein in bones, muscles, and all connective tissue.) Synthetic bulking materials, such as carbon-coated beads, are also used.
- The doctor passes the collagen-containing needle through a cystoscope, a tube that has been inserted into the urethra. The collagen can also be injected into the skin next to the sphincter.
- The injected collagen tightens the seal of the sphincter by adding bulk to the surrounding tissue.
- The procedure takes about 20 - 40 minutes, and most people can go home immediately afterward.
- Two or three additional injections may be needed to achieve satisfactory results.
Postoperative Care. People may experience immediate improvement followed by a temporary relapse after a week or so. Patients must be taught to use a catheter tube for withdrawing urine for a few days following the procedure. In general, it takes about a month for the full benefits to be apparent.
Complications.
- There is a risk for infection and urinary retention, although these conditions are temporary.
- The procedure may not be appropriate for patients with certain heart conditions.
Duration of Effectiveness. Collagen is absorbed over time, so injections generally need to be repeated every 6 - 18 months.
Sacral Neurostimulation
The sacral nerves, located near the sacrum (“tail bone”), appear to play an important role in regulating bladder control. A sacral nerve stimulation system (InterStim) may help some patients with urge incontinence. The system uses an implanted device to send electrical pulses to the sacral nerves to help retrain them. InterStim is reserved for the treatment of urinary retention and the symptoms of overactive bladder in patients who have failed or cannot tolerate less invasive treatments.
Complications include infection, lower back pain, and pain at the implant site. The system, however, does not cause nerve damage and can be removed at any time.
Patients have reported improvement in the frequency and volume of urination, as well as the intensity of urgency and their quality of life.
Lifestyle Changes
Hygiene Tips
Keeping Skin Clean. Proper hygiene is essential for patients with incontinence.
To avoid skin irritation and infection associated with incontinence, keep the area around the urethra clean. The following tips may be helpful:
- After a urinary accident, clean any affected areas right away.
- When bathing, use warm water and don't scrub forcefully; hot water and scrubbing can injure the skin.
- Cleansers are available that are specially created for incontinence and allow frequent cleansing without over-drying or causing irritation to the skin. Most do not have to be rinsed off; the area is simply wiped with a cloth.
- After bathing, apply a moisturizer plus a barrier cream. Barrier creams include petroleum jelly, zinc oxide, cocoa butter, kaolin, lanolin, or paraffin. These products are water repellent and protect the skin from urine.
- Anti-fungal creams that contain miconazole nitrate are u+
- sed for yeast infections.
Preventing or Reducing Odor. Certain methods may help reduce odor from accidents. They include:
- Deodorizing tablets can be taken by mouth or used in appliances.
- Drinking more water, not less, will also reduce odors. Drinking more water may actually help reduce leakage, too.
- To remove odors from mattresses, use a solution of equal parts vinegar to water. Once the mattress has dried, apply baking soda on the stain, rub it in, and then vacuum it off.
Dietary Considerations
Diet and Weight Control. In women, pelvic floor muscle tone weakens with significant weight gain. Weight loss can help reduce the frequency of urinary incontinence episodes in overweight women. Women should eat healthy foods in moderation and exercise regularly. Constipation can worsen urinary incontinence, so diets should be high in fiber, fruits, and vegetables.
Fluid Intake. A common misconception among people with incontinence is that drinking less water will prevent accidents. In reality, limiting fluid intake has the following effects:
- The lining of the urethra and bladder becomes irritated, which may actually increase leakage.
- Concentrated urine also has a stronger pungency, so drinking plenty of fluids can help reduce odor.
People with incontinence, however, should stop drinking beverages 2 - 4 hours before going to bed, particularly those who experience leakage or accidents during the night.
Fluid and Food Restrictions. A number of foods and beverages may increase incontinence. People who drink caffeinated or alcoholic beverages should try eliminating them to see if incontinence improves.
Considerations for Exercising
Sometimes otherwise healthy adults stop exercising because of leakage. There are a number of methods for preventing or stopping leakage during exercise. The following are some tips:
- Limit fluid intake before exercising (but be sure not to become dehydrated)
- Urinate frequently, including right before exercise
- Women can try wearing pads or urethral inserts
Urinary Incontinence Products
Many products are available to help patients avoid embarrassment and prevent leakage.
Absorbent Pads and Protective Undergarments
A variety of absorbent pads and undergarments are quite effective in catching spills and leaks. Newer types of pads are thin enough to be worn undetected, and a spare can be hidden in a purse or pocket. Many undergarments developed for incontinence are almost indistinguishable from regular briefs and underpants.
For men, drip collectors are available which can be worn under briefs and are not noticeable under normal clothing. Lined with absorbent material, the pouch-like collector surrounds the penis or scrotum and is fastened with a belt or pins.
All absorbent undergarments should be changed when wet to limit problems of chafing or infection.
External Devices
Self-Adhesive Foam Pads. Foam pads with an adhesive coating are available for women with stress incontinence. They work as follows:
- The pad is placed over the opening of the urethra where it creates a seal, preventing leakage.
- It is removed before urinating and replaced with a new one afterward.
- The pad can be worn up to 5 hours a day and through the night.
- It can be used during physical activity, although it may change position during vigorous exercise.
- It should not be worn during sexual intercourse.
Adhesive pads should not be used by women with the following conditions:
- Urinary tract or vaginal infections
- Urge or other forms of nonstress incontinence
- A history of surgery for incontinence
Urethral Caps. Small silicone caps that use suction to adhere to the urethral opening are also an option for women. These caps may be uncomfortable for some women, and side effects can include irritation and urinary tract infections.
Penile Clamps. The penile clamp is a hinged V-shaped external device that has two foam rubber pads which fit over the penis. When it is locked in place, it helps prevent dribbling. To urinate, the man releases the clamp.
Internal Devices
Vaginal Pessaries. Vaginal pessaries are devices inserted into the vagina that support the inside of the vaginal walls. Pessaries are usually made of silicon and come in various forms, including donut or cube-shapes. They must be fitted by a health professional and are effective for vaginal prolapse or other vaginal structural problems. Serious complications are rare but can occur if the pessary is not replaced periodically.
Urethral Tubes. Silicone tubes or sleeves that fit into the urethral opening are also available, although they are rarely recommended. When the tube is inserted into the urethra, the sleeve conforms to its shape and creates a seal at the bladder neck, preventing leakage. It is intended for one-time use and is replaced after voiding.
Catheters and Collection Devices
A catheter is a slim flexible tube inserted into the urethra. They are mainly used for cases of severe urge incontinence.
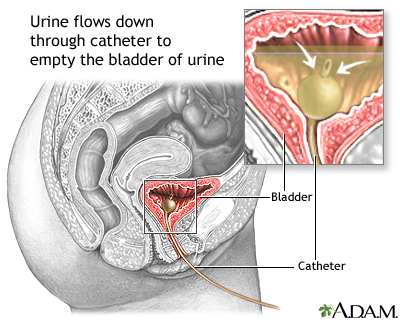
Temporary Catheterization. For people who are still active, catheterization is often very distressing. If possible, temporary, also called intermittent, catheterization is usually the best choice. Patients insert the catheter tube into their urethras, generally every 3 - 4 hours. This type of catheterization carries few risks and empties the bladder completely. Some patients report that they can maintain an active life with no significantly increased risk for infection with some simple precautions:
- Sterilize catheters at home.
- Use a zip lock plastic bag for carrying them when leaving home.
- Use another plastic bag for antiseptic cleansing solution.
- When using public bathrooms, wash before and after catheterization. Touch as few places in the bathroom as possible.
Permanent Catheterization. People who are mentally or physically incapable of self-catheterization may need permanent catheterization.
- The permanent catheter is inserted by a doctor or nurse into the opening of the bladder and a cuff is inflated to hold the tube in place. (A suprapubic tube may be recommended for long-term use. It is an indwelling catheter that is surgically placed directly into the bladder through the abdomen. The catheter is inserted above the pubic bone.)
- Urine drains to an external collection device, which is generally strapped to the leg and must be emptied periodically.
Nonsurgical catheterization procedures are generally not painful, but there is a substantial increased risk of infection. Many doctors feel that the catheter is overused, especially in the elderly.
External Collection Devices. External catheter and collection devices include:
- Condom catheters. Condom catheters are much more satisfactory than standard catheters for many male patients, although there is more spillage. The condom is worn all day and at night it is removed and washed for reuse the next day.
- Collection devices attached to the leg. For chronic or severe incontinence, collective devices drain urine into a bag that is attached to the lower leg and emptied periodically. These are generally more successful for men than women. Urine can be funneled into the tube by a pouch surrounding the penis. The positioning of the collecting device is difficult for women, and more accidents occur. For both men and women, irritation of the area around the urethral opening is a problem, since urine is in contact with the area for long periods.
Resources
- www.nafc.org -- National Association for Continence
- www.simonfoundation.org -- The Simon Foundation for Continence
- www.kidney.niddk.nih.gov -- National Kidney and Urologic Diseases Information
- www.acog.org -- American College of Obstetricians and Gynecologists
- www.urologyhealth.org -- Urology Health from the American Urological Association
References
Albo ME, Richter HE, Brubaker L, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med. 2007 May 24;356(21):2143-2155. Epub 2007 May 21.
American Urological Association. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. May 2012.
Anger JT, Weinberg A, Suttorp MJ, Litwin MS, Shekelle PG. Outcomes of intravesical botulinum toxin for idiopathic overactive bladder symptoms: a systematic review of the literature. J Urol. 2010 Jun;183(6):2258-64. Epub 2010 Apr 18.
Deng DY. Urinary incontinence in women. Med Clin North Am. 2011 Jan;95(1):101-9.
Dmochowski RR, Blaivas JM, Gormley EA, Juma S, Karram MM, Lightner DJ, et al. Update of AUA guideline on the surgical management of female stress urinary incontinence. J Urol. 2010 May;183(5):1906-14. Epub 2010 Mar 29.
Fader M, Cottenden AM, Getliffe K. Absorbent products for moderate-heavy urinary and/or faecal incontinence in women and men. Cochrane Database Syst Rev. 2008 Oct 8;(4):CD007408.
Hay-Smith J, Morkved S, Fairbrother KA, Herbison GP. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2008 Oct 8;(4):CD007471.
Herbison GP, Arnold EP. Sacral neuromodulation with implanted devices for urinary storage and voiding dysfunction in adults. Cochrane Database Syst Rev. 2009 Apr 15;(2):CD004202
Holroyd-Leduc JM, Tannenbaum C, Thorpe KE, Straus SE. What type of urinary incontinence does this woman have? JAMA. 2008 Mar 26;299(12):1446-56.
Imamura M, Abrams P, Bain C, Buckley B, Cardozo L, Cody J, et al. Systematic review and economic modelling of the effectiveness and cost-effectiveness of non-surgical treatments for women with stress urinary incontinence. Health Technol Assess. 2010 Aug;14(40):1-188, iii-iv.
Landefeld CS, Bowers BJ, Feld AD, Hartmann KE, Hoffman E, Ingber MJ, et al. National Institutes of Health state-of-the-science conference statement: prevention of fecal and urinary incontinence in adults. Ann Intern Med. 2008 Mar 18;148(6):449-58. Epub 2008 Feb 11.
Lee JH, Gomez S, Jankowski TA. FPIN’s clinical inquiries: hormone therapy for postmenopausal women with urinary incontinence. Am Fam Physician. 2011 Jul 1;84(1):1-2.
Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: US Government Printing Office, 2007; NIH Publication No. 07–5512.
Marinkovic SP, Rovner ES, Moldwin RM, Stanton SL, Gillen LM, Marinkovic CM. The management of overactive bladder syndrome. BMJ. 2012 Apr 17;344:e2365. doi: 10.1136/bmj.e2365.
North American Menopause Society. The 2012 hormone therapy position statement of: The North American Menopause Society. Menopause. 2012 Mar;19(3):257-71.
Nygaard I. Clinical practice. Idiopathic urgency urinary incontinence. N Engl J Med. 2010 Sep 16;363(12):1156-62.
Richter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010 Jun 3;362(22):2066-76. Epub 2010 May 17.
Rogers RG. Clinical practice. Urinary stress incontinence in women. N Engl J Med. 2008 Mar 6;358(10):1029-36.
Rogers RG. What's best in the treatment of stress urinary incontinence? N Engl J Med. 2010 Jun 3;362(22):2124-5. Epub 2010 May 17.
Shamliyan TA, Kane RL, Wyman J, Wilt TJ. Systematic review: randomized, controlled trials of nonsurgical treatments for urinary incontinence in women. Ann Intern Med. 2008 Mar 18;148(6):459-73. Epub 2008 Feb 11.
Shamliyan T, Wyman JF, Ramakrishnan R, Sainfort F, Kane RL. Benefits and harms of pharmacologic treatment for urinary incontinence in women: a systematic review. Ann Intern Med. 2012 Jun 19;156(12):861-74, W301-10.
Subak LL, Wing R, West DS, Franklin F, Vittinghoff E, Creasman JM, et al. Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med. 2009 Jan 29;360(5):481-90.
Thirugnanasothy S. Managing urinary incontinence in older people. BMJ. 2010 Aug 9;341:c3835. doi: 10.1136/bmj.c3835.
Wing RR, Creasman JM, West DS, Richter HE, Myers D, Burgio KL, et al. Improving urinary incontinence in overweight and obese women through modest weight loss. Obstet Gynecol. 2010 Aug;116(2 Pt 1):284-92.
|
Review Date:
9/25/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M. Health Solutions, Ebix, Inc. |







